Decoding MSSA Bacteremia: Understanding ICD-10 Codes and Their Significance
Methicillin-sensitive Staphylococcus aureus (MSSA) bacteremia is a bloodstream infection caused by the MSSA bacteria. Accurate diagnosis and coding are crucial for effective treatment and tracking of this condition. One of the key tools in this process is the International Classification of Diseases, Tenth Revision (ICD-10). This article provides a comprehensive overview of MSSA bacteremia, focusing on the relevant ICD-10 codes and their clinical significance.
What is MSSA Bacteremia?
Bacteremia, in simple terms, means the presence of bacteria in the bloodstream. When this condition is caused by Methicillin-sensitive Staphylococcus aureus, it is classified as MSSA bacteremia. Staphylococcus aureus is a common bacterium that can reside on the skin and in the nose without causing harm. However, when it enters the bloodstream, it can lead to severe infections.
MSSA is a strain of Staphylococcus aureus that remains susceptible to common antibiotics like methicillin and its derivatives. This is in contrast to Methicillin-resistant Staphylococcus aureus (MRSA), which is resistant to these antibiotics and often more difficult to treat. [See also: MRSA Treatment Options]
Risk Factors for MSSA Bacteremia
Several factors can increase the risk of developing MSSA bacteremia:
- Compromised Immune System: Individuals with weakened immune systems due to conditions like HIV/AIDS, cancer, or immunosuppressant medications are more susceptible.
- Recent Surgery or Invasive Procedures: Surgical incisions, catheters, and other invasive procedures can provide entry points for the bacteria.
- Intravenous Drug Use: Injecting drugs can introduce bacteria directly into the bloodstream.
- Chronic Conditions: Conditions like diabetes and kidney disease can increase the risk of infection.
- Skin Infections: Existing skin infections, such as cellulitis or abscesses, can sometimes lead to bacteremia.
Symptoms of MSSA Bacteremia
The symptoms of MSSA bacteremia can vary depending on the severity of the infection and the individual’s overall health. Common symptoms include:
- Fever
- Chills
- Rapid heart rate
- Low blood pressure
- Confusion or altered mental status
- Pain or swelling at the site of infection (if present)
In severe cases, MSSA bacteremia can lead to sepsis, a life-threatening condition characterized by widespread inflammation and organ damage.
ICD-10 Codes for MSSA Bacteremia
The ICD-10 coding system is used to classify and code diagnoses, symptoms, and procedures. For MSSA bacteremia, the primary ICD-10 code is crucial for accurate billing, data collection, and public health reporting. Several codes might be relevant depending on the specific presentation and complications of the infection.
Primary Code
The most relevant and commonly used ICD-10 code for MSSA bacteremia is:
- A41.01: Sepsis due to Methicillin susceptible Staphylococcus aureus
This code specifically identifies that the sepsis is caused by MSSA. Sepsis is a serious complication of bacteremia, making this a critical code to use when applicable.
Additional Codes
In addition to the primary code, other ICD-10 codes may be used to provide further specificity and detail about the patient’s condition. These codes can include:
- B95.61: Methicillin susceptible Staphylococcus aureus [MSSA] as the cause of diseases classified elsewhere. This code should be used to identify MSSA as the causative organism when the infection manifests in a specific organ or site.
- R65.20: Severe sepsis without septic shock. This code is used when the patient exhibits signs of severe sepsis but has not yet developed septic shock.
- R65.21: Severe sepsis with septic shock. This code is used when the patient has progressed to septic shock, a life-threatening condition characterized by dangerously low blood pressure and organ dysfunction.
- Codes for specific organ involvement (e.g., pneumonia, endocarditis, osteomyelitis) if the MSSA bacteremia has led to complications in those areas. For example, if the patient develops pneumonia due to MSSA bacteremia, a code for pneumonia would also be included.
Importance of Accurate ICD-10 Coding
Accurate ICD-10 coding for MSSA bacteremia is essential for several reasons:
- Proper Reimbursement: Accurate coding ensures that healthcare providers receive appropriate reimbursement for the services they provide.
- Data Collection and Analysis: ICD-10 codes are used to track the incidence and prevalence of diseases, including MSSA bacteremia. This data is crucial for public health surveillance and research efforts.
- Quality Improvement: By tracking outcomes associated with different ICD-10 codes, healthcare organizations can identify areas for improvement in patient care.
- Clinical Decision Support: ICD-10 codes can be used to trigger alerts and reminders in electronic health records, helping clinicians make informed decisions about patient management.
Diagnosis and Treatment of MSSA Bacteremia
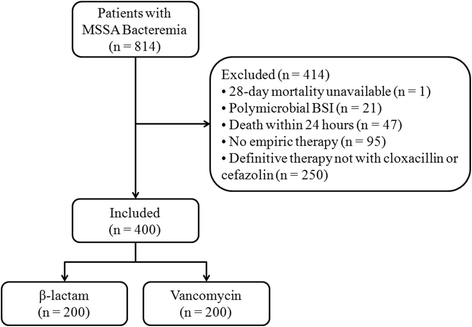
Diagnosing MSSA bacteremia typically involves blood cultures to identify the presence of Staphylococcus aureus in the bloodstream. Once the diagnosis is confirmed, treatment usually involves intravenous antibiotics. The choice of antibiotic depends on the susceptibility of the MSSA strain and the patient’s overall health.
Commonly used antibiotics for treating MSSA bacteremia include:
- Penicillinase-resistant penicillins: such as nafcillin or oxacillin
- First-generation cephalosporins: such as cefazolin
- Clindamycin: (though resistance can be an issue)
- Vancomycin: (often used if there are concerns about penicillin allergies or resistance)
The duration of antibiotic therapy depends on the severity of the infection and the presence of any complications. In some cases, surgical drainage of abscesses or removal of infected devices (e.g., catheters) may also be necessary.
Prevention of MSSA Bacteremia
Preventing MSSA bacteremia involves implementing strategies to reduce the risk of Staphylococcus aureus infections. These strategies include:
- Hand Hygiene: Frequent handwashing with soap and water or using alcohol-based hand sanitizers is crucial for preventing the spread of bacteria.
- Proper Wound Care: Keeping wounds clean and covered can help prevent infection.
- Catheter Management: Following strict protocols for inserting and maintaining catheters can reduce the risk of bloodstream infections.
- Decolonization Strategies: In some cases, decolonization strategies, such as using mupirocin nasal ointment or chlorhexidine washes, may be used to reduce the risk of Staphylococcus aureus carriage.
The Role of Infection Control Professionals
Infection control professionals play a vital role in preventing and managing MSSA bacteremia in healthcare settings. They develop and implement policies and procedures to minimize the risk of infection, monitor infection rates, and educate healthcare staff about infection control practices. [See also: Infection Control Best Practices]
Their responsibilities include:
- Surveillance of healthcare-associated infections
- Implementation of infection control measures
- Education and training of healthcare personnel
- Collaboration with other healthcare professionals to improve patient safety
MSSA Bacteremia in Specific Populations
Certain populations are at higher risk for developing MSSA bacteremia and require special consideration.
Neonates
Newborn infants, especially premature infants, are particularly vulnerable to MSSA bacteremia due to their immature immune systems. Infections in neonates can be severe and require prompt treatment.
Elderly
Older adults are also at increased risk due to age-related changes in immune function and the presence of underlying medical conditions. They may also have atypical presentations of infection, making diagnosis more challenging.
Patients with Indwelling Devices
Patients with central venous catheters, prosthetic joints, or other indwelling devices are at higher risk for bloodstream infections. Careful management of these devices is essential to prevent infection.
Future Directions in MSSA Bacteremia Research
Ongoing research efforts are focused on developing new strategies for preventing and treating MSSA bacteremia. These efforts include:
- Developing new antibiotics to combat resistant strains of Staphylococcus aureus
- Improving diagnostic methods for early detection of bacteremia
- Developing vaccines to prevent Staphylococcus aureus infections
- Exploring novel therapeutic approaches, such as immunotherapy
Conclusion
MSSA bacteremia is a serious infection that requires prompt diagnosis and treatment. Understanding the relevant ICD-10 codes, risk factors, symptoms, and prevention strategies is crucial for healthcare professionals. By implementing effective infection control measures and staying informed about the latest advances in research, we can improve outcomes for patients with MSSA bacteremia. Accurate coding related to MSSA bacteremia, specifically using ICD-10, is paramount. The correct ICD-10 code for MSSA bacteremia ensures proper billing and tracking. Remember, MSSA bacteremia ICD-10 coding directly impacts data analysis. Effective management of MSSA bacteremia relies on correct ICD-10 application. The term MSSA bacteremia is clearly defined by its ICD-10 code. For accurate reporting, always verify the correct ICD-10 for MSSA bacteremia. The presence of MSSA bacteremia is confirmed via blood culture and subsequently coded using ICD-10. Understanding the ICD-10 code for MSSA bacteremia is crucial for healthcare providers. MSSA bacteremia ICD-10 is a critical component of patient documentation. Proper ICD-10 coding of MSSA bacteremia contributes to quality improvement initiatives. MSSA bacteremia and its ICD-10 classification play a role in clinical decision support. Monitoring MSSA bacteremia trends involves analyzing ICD-10 coded data. [See also: Importance of Accurate Medical Coding]
