Lobotomy, Memory Loss, and the Point of No Return: Understanding the Consequences
The history of medicine is filled with procedures once hailed as revolutionary, only to be later understood as deeply flawed and even harmful. Among these, the lobotomy stands out as a particularly stark example. This neurosurgical procedure, intended to alleviate severe mental illness, often resulted in devastating side effects, most notably profound memory loss. Examining the connection between lobotomy, memory loss, and the concept of a ‘point of no return‘ provides critical insights into the ethics of medical innovation and the importance of understanding the long-term consequences of medical interventions.
The Rise and Fall of the Lobotomy
The lobotomy gained prominence in the mid-20th century as a treatment for a variety of psychiatric disorders, including schizophrenia, severe depression, and anxiety. Developed primarily by Portuguese neurologist António Egas Moniz, who later received the Nobel Prize in Physiology or Medicine in 1949 for his discovery of the therapeutic value of leucotomy in certain psychoses, the procedure involved severing connections in the brain’s prefrontal cortex. The initial rationale was that by disrupting these connections, the procedure could reduce the intensity of emotional disturbances and restore patients to a more manageable state. [See also: History of Psychiatric Treatment]
The procedure was popularized in the United States by Walter Freeman, who developed the transorbital lobotomy, a less invasive but arguably more brutal method performed by inserting an ice pick-like instrument through the eye socket to sever the frontal lobe connections. This technique allowed for faster and more widespread application, leading to tens of thousands of lobotomies performed in the US and other countries.
Memory Loss: A Devastating Consequence
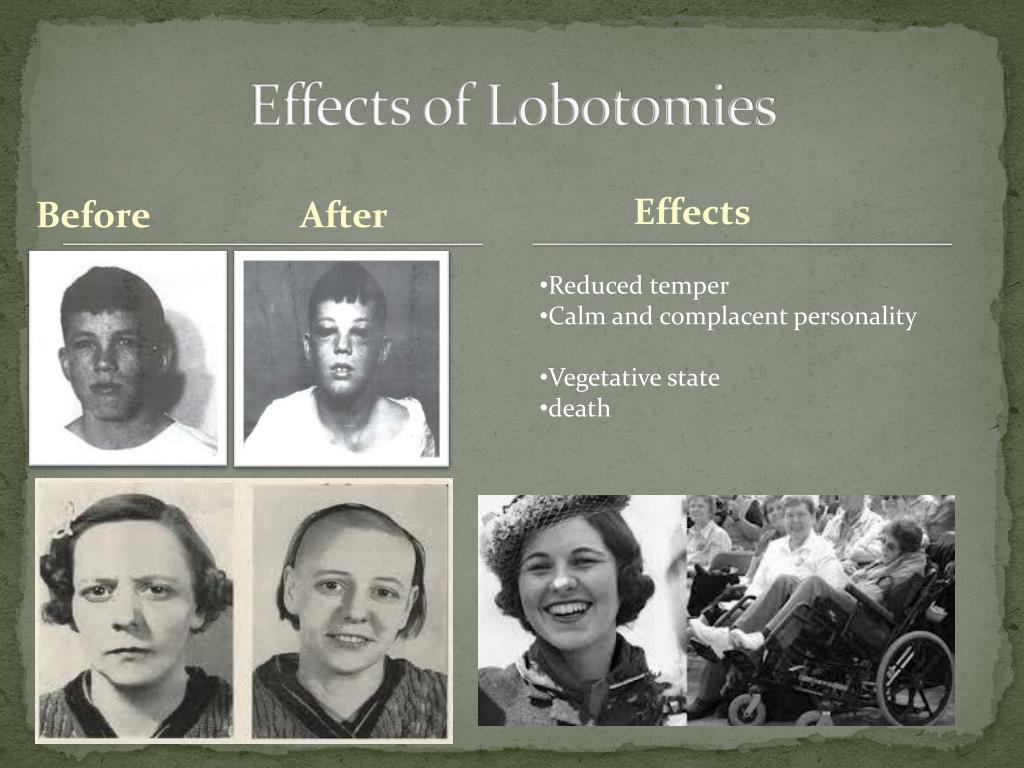
While some patients experienced a reduction in their symptoms, the lobotomy often came at a significant cost. One of the most common and devastating side effects was memory loss. The prefrontal cortex plays a crucial role in higher cognitive functions, including working memory, decision-making, and personality. Severing these connections disrupted these functions, leading to a range of cognitive impairments. Patients often experienced difficulties with short-term memory, long-term memory, and the ability to form new memories. This memory loss could range from mild forgetfulness to severe amnesia, profoundly impacting their ability to function in daily life.
Beyond memory loss, other common side effects included personality changes, emotional blunting, reduced initiative, and impaired judgment. Many patients became apathetic and dependent, losing their ability to live independently. The procedure essentially traded one set of problems for another, often leaving individuals in a worse state than before. [See also: The Ethics of Medical Procedures]
The Point of No Return: Assessing Irreversible Damage
The concept of a ‘point of no return‘ is particularly relevant when considering the lobotomy. Because the procedure involved irreversible damage to brain tissue, the consequences were often permanent. Once the connections in the prefrontal cortex were severed, there was no way to undo the damage. This meant that any memory loss or personality changes resulting from the lobotomy were likely to be lifelong. The ‘point of no return‘ had been crossed, leaving patients and their families to cope with the devastating aftermath.
The irreversible nature of the procedure raised serious ethical questions about informed consent and the balance between potential benefits and risks. In many cases, patients were not fully informed about the potential consequences of the lobotomy, and their families may have been pressured to consent to the procedure in the hope of alleviating their loved one’s suffering. The lack of effective treatments for severe mental illness at the time contributed to the widespread acceptance of the lobotomy, despite its significant risks. [See also: Informed Consent in Medical Treatment]
Ethical Considerations and Lessons Learned
The history of the lobotomy serves as a cautionary tale about the importance of rigorous scientific evaluation and ethical oversight in medical innovation. The widespread adoption of the procedure without sufficient evidence of its long-term efficacy and safety highlights the dangers of prioritizing immediate solutions over careful research and patient well-being. The devastating consequences of memory loss and other side effects underscore the need for a more nuanced understanding of the brain and the potential impact of surgical interventions.
Modern neuroscience has made significant advances in understanding the complexities of the brain and the mechanisms underlying mental illness. Today, a range of treatments are available, including medication, psychotherapy, and neurostimulation techniques, that offer more targeted and less invasive approaches to managing psychiatric disorders. The development of these treatments has been informed by the lessons learned from the lobotomy era, emphasizing the importance of evidence-based practice and a commitment to minimizing harm. The exploration of treatments must consider memory loss as a potential side effect.
The Legacy of the Lobotomy
While the lobotomy is now largely discredited and rarely performed, its legacy continues to shape the field of mental health. The procedure serves as a reminder of the potential for medical interventions to cause unintended harm and the importance of prioritizing patient safety and well-being. The stories of individuals who underwent lobotomies and suffered from memory loss and other debilitating side effects serve as a powerful testament to the need for ethical and responsible medical practice. Understanding the long term effects of neurological procedures is critical to ensuring that we do not reach a point of no return for patients.
The impact of the lobotomy extended beyond the individual patients who underwent the procedure. Families and communities were also affected by the devastating consequences of memory loss and personality changes. The financial and emotional burden of caring for individuals who had undergone lobotomies often fell on family members, who struggled to cope with the challenges of providing long-term care. The societal impact of the lobotomy serves as a reminder of the interconnectedness of individual health and community well-being.
Moving Forward: A Commitment to Ethical and Evidence-Based Practice
As we continue to advance our understanding of the brain and develop new treatments for mental illness, it is essential to remain mindful of the lessons learned from the lobotomy era. A commitment to ethical and evidence-based practice is crucial for ensuring that medical interventions are both effective and safe. This includes conducting rigorous scientific research to evaluate the long-term efficacy and safety of new treatments, obtaining informed consent from patients, and prioritizing patient well-being above all else. The potential for memory loss must always be considered.
The history of the lobotomy also underscores the importance of humility in medicine. Medical knowledge is constantly evolving, and what is considered an acceptable treatment today may be viewed differently in the future. It is essential to remain open to new evidence and to be willing to re-evaluate existing practices in light of new information. This requires a willingness to challenge assumptions and to engage in ongoing dialogue about the ethical and social implications of medical innovation. The lobotomy highlighted a clear point of no return for many patients.
In conclusion, the story of the lobotomy and its association with memory loss serves as a powerful reminder of the complexities and challenges of medical innovation. By understanding the history of this procedure and the lessons learned from its widespread use, we can work towards a future where medical interventions are both effective and ethically sound. The concept of a ‘point of no return‘ should always be at the forefront of our minds when considering medical procedures with potentially irreversible consequences. The lasting impact on patients’ memory underscores the need for cautious and ethical medical practice. The risks of memory loss are a critical consideration. The procedure serves as a reminder of the potential for medical interventions to cause unintended harm, and the importance of prioritizing patient safety and well-being. The severe memory loss experienced by many patients highlights the need for careful consideration of the potential risks and benefits of any medical intervention. The dangers of lobotomy and associated memory loss are a key part of medical history. The ethical issues surrounding lobotomy and the resulting memory loss are still relevant today. The long-term effects of lobotomy, particularly memory loss, were often not fully understood at the time. The irreversible nature of lobotomy meant that patients often reached a point of no return. The correlation of lobotomy and memory loss shows the importance of ethical considerations.
